In today’s healthcare landscape, academic medical centers (AMCs) play a critical role in advancing research, education, and patient care.
Those who are familiar with AMCs understand the opportunities afforded to the community through these unique healthcare models. However, educating potential donors on the importance of AMCs and addressing the other challenges facing today’s academic healthcare organizations can be tricky.
In this guide, we review everything you need to know to effectively engage donors in fundraising, communications, strategic planning, and relationship building to support the mission of academic medical centers.
- What is an Academic Medical Center?
- Three Primary roles of Academic Medical Centers
- How Academic Medical Centers Empower Philanthropy
- 7 Ways to Leverage the Benefits of Academic Medical Centers
- Addressing the Challenges of Academic Medical Centers
- Tips for Fundraising at Academic Medical Centers
What is an Academic Medical Center?
To understand the ways to leverage your unique position as an AMC, you must first define and understand exactly what makes an AMC, an AMC.
An academic medical center is generally defined as a medical facility that is associated with a medical school or university and provides clinical care, education, and research opportunities for medical students, residents, and fellows. AMCs typically focus on advancing medical knowledge through research, clinical trials, and other innovative practices. They often offer specialized and high-quality care and have a reputation for being at the forefront of medical research and technology.
In addition to providing patient care and education, AMCs often play a crucial role in developing and training the next generation of medical professionals and conducting research that can lead to new treatments and cures for diseases.
AMCs are the training grounds for emerging physicians, the birthplaces of new discoveries, and the providers of the most complex life-saving care. And, as the COVID-19 pandemic revealed, they are a critical component of our public health response.
Ultimately, one of the most important things you can do as a fundraiser within an AMC is to never make assumptions that your donors—and even your colleagues—fully understand what it means to be an AMC. Continually reinforcing the power and impact that AMCs have on our healthcare landscape and the unique nature of an AMC model is important throughout your tenure as a development professional. Be loud, be proud, and always keep AMC points of pride at the forefront of your messaging.
Three Primary Roles of Academic Medical Centers
AMCs provide many benefits to patients, the community, and the global healthcare landscape. There are three main reasons why AMCs are so vital to healthcare.
1. Creating Medical Research Breakthroughs
Research and innovation are at the core of AMCs. From NICUs to cancer research that have saved more than 2.5 million people in the past 30 years alone, it all starts in academic medicine.
2. Shaping the Future of Medicine
More diverse medical teams make better decisions—and have better patient outcomes. AMCs work to ensure tomorrow’s doctors have the innovative training they need to improve health everywhere.
3. Advancing Patient Care
Academic medicine is where expert patient care and innovation come together to save lives. In fact, patients treated at teaching hospitals have higher odds of survival than at non-teaching hospitals.
How Academic Medical Centers Empower Philanthropy
With best-in-class patient care, cutting-edge research, and top-tier education, AMCs provide many benefits. But when philanthropy is added to the formula, the magic really happens! Philanthropy can elevate the profile and impact of AMCs and provide funding for breakthroughs that wouldn’t be possible without the expertise of the AMC combined with the passion of a donor.
As a fundraiser, you can set the sights of both leadership and philanthropists by highlighting four major ways for gifts to support healthcare:
Funding Research
Philanthropy provides critical funding for research at AMCs, which can help accelerate medical breakthroughs, improve patient outcomes, and address healthcare challenges. Research funding can support projects ranging from basic science research to clinical trials and translational research. Additionally, donors may be able to provide seed funding for the early discovery work that many government grants do not support. By doing so, researchers may be able to turn an experimental idea into a lifesaving cure-all due to a donor’s gift that is then leveraged for larger grant dollars. The idea of utilizing donors’ gifts in this way can be very inspirational. We recommend that this becomes a routine talking point when discussing research support.
Enhancing Patient Care
Donor support of new programs, technologies, and facilities can enhance patient care at AMCs. Donations can help fund the purchase of new equipment, the construction of new buildings or wings, and the hiring of additional staff, among other things.
Addressing Health Disparities
The role of philanthropy is important when addressing health disparities by bolstering programs and initiatives that focus on underserved populations. This can include outreach and education programs, community-based research, and initiatives to increase access to healthcare services for vulnerable populations.
Providing Scholarships and Fellowships
Philanthropy can also support the education and training of the next generation of healthcare professionals by funding scholarships and fellowships. This can help attract and retain top talent and also help ensure that patients receive the highest quality care from well-trained and knowledgeable providers.
7 Ways to Leverage the Benefits of Academic Medical Centers
There are many benefits of AMCs and plenty of opportunities for you to leverage as a fundraising professional. Giving donors a thorough understanding of these benefits and the ways in which philanthropy can impact healthcare is vital to advancing the mission of your AMC.
Better Patient Outcomes
A study published in JAMA found that patients treated at a major teaching hospital have up to 20 percent higher odds of survival, compared to those treated at non-teaching hospitals. After adjusting for patient and hospital characteristics, the same study found high-severity patients had 7 percent lower odds of 30-day mortality, medium-severity patients had 13 percent lower odds, and low-severity patients had 17 percent lower odds compared to similar patients at non-teaching facilities.
“Taken together, these findings suggest that efforts to limit care at academic medical centers have the potential to lead to worse outcomes, as mortality rates for even low-severity patients seem to be lower at the centers,” the study authors wrote.
Cutting-Edge Research
Research covers a vast array of areas and is typically thought of as a “bench to bedside and back again” approach at many AMCs. AMC research can be considered a three-legged stool consisting of basic research, translational research, and clinical trials.
Basic Research
Basic science is anything but basic—it is the root of all healthcare breakthroughs. Basic science includes disciplines such as biochemistry, microbiology, physiology, and pharmacology. At its core, basic science involves laboratory studies with cell cultures, animal studies, or physiological experiments. Basic science research focuses on how the body works in both health and in illness and is rooted in building hypotheses to be tested and revised.
Translational Research
Translational research takes basic science to the next level. Once fundamental principles of biological processes are understood, these discoveries can be applied to or translated into direct application to patient care.
Translational research includes:
- Preclinical Research: Preclinical research connects the basic science of disease with human medicine. During this stage, scientists develop model interventions to further understand the basis of a disease or disorder and find ways to treat it. Testing is carried out using cell or animal models of disease; samples of human or animal tissues; or computer-assisted simulations of drug, device, or diagnostic interactions within living systems.
- Clinical Research: Clinical research includes studies to better understand a disease in humans and relate this knowledge to findings in cell or animal models, testing and refinement of new technologies in people, testing of interventions for safety and effectiveness in those with or without disease, behavioral and observational studies, and outcomes and health services research. The goal of many clinical trials is to obtain data to support regulatory approval for an intervention.
- Clinical Implementation: The clinical implementation stage of translational science involves the adoption of interventions that have been demonstrated to be useful in a research environment into routine clinical care for the general population. This stage also includes implementation research to evaluate the results of clinical trials and to identify new clinical questions and gaps in care.
- Public Health: In this stage of translation, researchers study health outcomes at the population level to determine the effects of diseases and efforts to prevent, diagnose, and treat them. Findings help guide scientists working to assess the effects of current interventions and to develop new ones.
Clinical Trials
Clinical trials are one of the most well-known benefits of seeking care at an AMC and one of the reasons that many donors support AMCs.
- Allow patients to play an active role in their own healthcare.
- Gain access to new research treatments before they are widely available.
- Increase the options for treatment when standard therapy has failed.
- Provide patients with expert medical care at leading healthcare facilities during the trial.
- Help others by contributing to the advancement of medical knowledge.
Drug Discovery
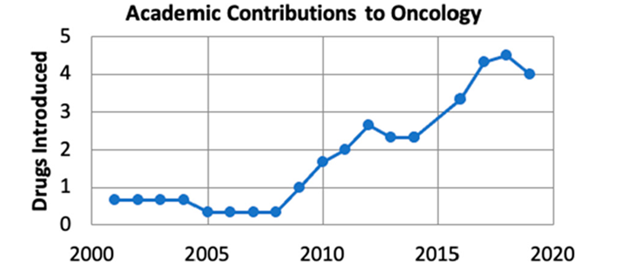
Thanks to the three-legged stool of basic science, translational science, and clinical trials, AMCs are also able to discover or repurpose drugs that lead to new treatment options. Academic inventors or founders contributed to more than a quarter of all medicines approved from 2001 through 2019. Among the therapeutic areas, academic inventors contributed to more than a third (37%) of cancer medicines. Inventive academic contributions were particularly prominent for certain indications. For example, 80 percent of drugs developed for multiple myeloma from 2001 to 2019 had an academic inventor or founder, as did 67 percent of drugs approved for melanoma, 56 percent of lymphoma, and 50 percent of prostate cancer medicines.
Teaching the Next Generation
Teaching is one of the core tenets of an AMC. It is important to recognize that America is facing a healthcare worker shortage in the next decade, and AMCs are at the forefront of providing solutions.
According to the Association of American Medical Colleges (AAMC), America faces a shortage of up to 122,000 physicians by 2032, and one-third of doctors today are over the age of 65 and nearing retirement. The nation’s 154 accredited medical schools and more than 400 major teaching hospitals and health systems are combatting this issue every day. To help address the looming doctor shortage, the nation’s medical schools have increased class sizes, and 26 new medical schools have opened in the past decade. Altogether, these institutions have expanded enrollment by 30 percent to help ease the effects of the doctor shortage.
Along with educating more doctors, medical schools and teaching hospitals are training doctors in new ways and enhancing and refining curricula to ensure tomorrow’s healthcare professionals are getting the training they need to improve the overall health of our population. Examples include educating future doctors to address social determinants of health, responding to healthcare crises like the opioid epidemic, and providing care for ongoing healthcare needs such as obesity, smoking, diabetes, and heart disease.
Improving the Health and Well-Being of the Community
AMCs help the community in a myriad of ways, some of which are more obvious than others. AMCs operate 71 percent of accredited level-one trauma centers and 98 percent of the nation’s 43 comprehensive cancer centers. Teaching hospitals—which are only 5 percent of all hospitals in the United States—provide 69 percent of all burn unit beds, 63 percent of pediatric intensive care unit beds, 19 percent of all alcohol unit beds, and 24 percent of all inpatient psychiatric beds. AMCs also provide treatment for a disproportionately high percentage of Medicare and Medicaid beneficiaries as well as those who are uninsured.
Addressing Health Disparities
AMCs can play a significant role in addressing health disparities through research, education, and community engagement. Many of the nation’s medical schools and teaching hospitals also run innovative programs to address underlying social and economic factors in their communities that can lead to poor health. This includes providing access to healthy food, adequate housing, education, and transportation—all of which are social determinants of health.
Here are a few more examples of how AMCs address health disparities:
- Research: AMCs conduct research to understand the root causes of health disparities and develop interventions to address them. For instance, the University of California, San Francisco has established the Center for Vulnerable Populations to conduct research on health disparities affecting vulnerable populations, such as low-income individuals and communities of color.
- Education: AMCs train the next generation of healthcare providers to address health disparities. For example, the University of Michigan Medical School has a curriculum that includes training on health equity and social determinants of health.
- Community Engagement: AMCs work with communities to identify health disparities and develop interventions to address them. The University of Alabama at Birmingham has established the Office for Equity and Diversity to work with underserved communities and address health disparities.
- Health Policy: AMCs can influence health policy to address health disparities. The Harvard Medical School has established the Center for Primary Care to advocate for policies that promote health equity.
Economic Benefits
AMCs are powerful contributors to the economic health of their communities. One AAMC study showed that AMCs contributed more than $562B in value to the national economy in 2017 and supported more than 6.3 million U.S. jobs. Medical research was responsible for another 313,604 jobs and added $25.4B to local economies in 2017.
AMCs are often among the largest, if not the largest, employers in an area and typically employ a highly skilled workforce. AMCs also create jobs indirectly with vendors and suppliers, and many offer workforce development programs and career ladder options otherwise unavailable.
Addressing the Challenges of Academic Medical Centers
In addition to the many benefits and opportunities that AMCs afford, there are real challenges and misconceptions that must be addressed when speaking with donors and community members about AMCs.
Misconceptions and Fears
Given their unique nature, AMCs often have an air of mystery about them. What makes them so different than a local hospital? As you’ve read, there are many things! But given that these misconceptions may lead patients to choose other hospitals or donors to choose to give to other organizations addressing many of the same problems as AMCs, it is important that these notions be debunked quickly and directly.
Here are just a few examples of statements you may have heard or could hear in the future:
- “I don’t want to be a guinea pig!”
- Consider responding with, “Without clinical trials, today’s patients would be getting yesterday’s treatments, and there are so many great therapies afforded to us now. I hear your concern though, and I am not a medical professional. Please speak with your physician and express your fears about the possibility of a clinical trial. They will review all treatment options with you and can explain if and why a clinical trial may be a good option for you.”
- “A student doctor? No, thank you!”
- Consider responding with, “As an academic medical center, we are extremely fortunate to be training tomorrow’s physicians. The extensive training that they receive prepares them to deliver the very best patient care. There are also very experienced faculty members who are always working alongside residents. Please discuss your fears with a physician, and I am sure you will be comforted by knowing how much oversight our experienced professionals will have as a part of your care team.”
- “I’m not that sick. I don’t need a hospital like that.”
- Consider responding with, “We hear that often, but statistics show that patients have better outcomes at academic medical centers—even those patients who are not critically ill. We encourage you to have a consultation with one of our physicians to discuss your specific healthcare plan, and in partnership, you can determine if our hospital may be right for you.”
- “I like my community hospital, and it seems to be cheaper.”
- Consider responding with, “We encourage you to have a consultation with one of our physicians to determine if the course of treatment at our hospital may be right for you or if the standard course of care can be delivered at your community hospital. Your care team, including our financial support staff, will help you better understand your options and what is best for your health, your convenience, and your financial situation.”
It is important that a development officer never overstep their boundaries or areas of expertise—especially when discussing medical decisions—but since you may be confronted with these misconceptions while working alongside grateful patients, families, and concerned community members, it is important that you are prepared with answers. It is recommended that you listen to the patient’s or donor’s concerns and work with your medical leadership and faculty to understand how they may combat these misconceptions. Utilize the points of pride of your hospital and the information contained in this article to showcase the many benefits of AMCs.
Cost and Reimbursement
While we just reviewed many misconceptions about AMCs, it is important to understand that the cost of healthcare and reimbursement rates are very real issues that impact both the patients and AMCs.
AMCs have above-average costs for care due to their disproportionate share of uncompensated services they deliver and their staffing requirements. Additionally, payers may “nudge” patients to seek lower-cost facilities, and some insurance companies even exclude AMC facilities from narrow networks because they have higher costs.
It is important to note that many of the benefits of an AMC also create financial concerns for hospital leadership and management. AMCs receive lower Medicare and Medicaid reimbursements, and government funding for research has been greatly reduced in recent years. In today’s technology-savvy markets, increased telemedicine has decreased in-person consultations, which in turn has decreased revenue. Private systems are receiving more of the market share.
AMCs are reliant on government grants, philanthropy, and patient revenue but funding sources are uncertain and always subject to change. While these are very real challenges, it can be persuasive to address these issues with donors to help inspire philanthropy.
Tips for Fundraising at Academic Medical Centers
With a thorough understanding of the benefits and challenges facing AMCs, it is important to understand the ways in which you can impact philanthropy and leverage your messaging to increase support.
Communication Strategies and Tactics
Develop a clear message about your role as an AMC and share it broadly and in strategic one-on-one efforts. It is important that you first share within your organization and consider the following core groups for both input as well as approval:
- Your development teams
- Marketing and communications
- Can they partner with you on this?
- What materials and talking points do they already have?
- Your leaders
- Key clinicians and researchers
Develop a narrative about the innovations happening at your institution—what makes your AMC distinctive and invaluable to your patients and community. Ideally, your marketing and communications team can be key partners in this process. They may already have developed these materials.
Don’t forget your partners who make an AMC, an AMC—often, we use leadership, clinicians, and researchers to help us tell our compelling story to donors. Don’t leave them out! Educate them about how they can share their professional passion with donors and tie that into the greater aims of an AMC.
Understanding the Donor Populations of Academic Medical Centers
AMCs have the advantage of serving a community through patient care but helping the world through research and education. Because of this breadth, AMCs can connect with a wide spectrum of donor populations.
Four of them include:
- Patients and Families: Those who have experienced the care of the AMC firsthand and so want to give back.
- Former Learners: Many residents, fellows, and other learners build strong bonds with each other, their departments, and the institution. Those connections can last a lifetime and are worth cultivating.
- Research-Focused Funders: Individuals and foundations who care about research may want to support the research happening at your institution, even if they aren’t in your backyard.
- Community Members: AMCs may find that even community members without a strong healthcare tie to the institution may want to support it. They are grateful to have an anchor institution like an AMC in their community and want to ensure it stays strong.
Broad Communication Efforts
It is important to reinforce and repeat the messaging points about an AMC with the general public and donors alike. Consider weaving the AMC message throughout your website, publications, and direct marketing.
Here’s an example from an annual giving direct mailing:
“You can help us advance research, power innovation, support students in medical training, provide patient services for children and families, ease the journey of cancer patients, help us care for vulnerable populations across our region, and so much more.”
Additionally, videos are an impactful and visually appealing way to educate donors on what an AMC is and why your hospital is worthy of support. Consider all platforms and a multichannel approach to your broad communication strategies.
Academic Medical Center Donor Education as a Cultivation Strategy
Educating your donors about the power of AMCs can be a powerful cultivation tool. Demonstrate the power of research, education, and patient care through:
- Offering hands-on tours of research labs.
- Hearing from students.
- Talking to nurses about how they innovate to improve patient care.
- Attending a lecture or grand rounds.
- Meeting with a clinician who can talk about caring for patients, training residents, and researching an illness.
The Power of Academic Medical Centers and Solicitations
Ultimately, donors want to influence healthcare today and for the next generation. The power of AMCs is strong, and the ways in which you position your solicitations can have a great impact on the outcomes. Showcase the effect of your AMC in your community, your state, the nation, and the world. Be bold with your solicitation—as the mission of your AMC is certainly bold and worthy of support.
With the benefits and opportunities outlined here, along with your strong knowledge of your own hospital’s points of pride, you are poised to be successful and influence philanthropy—and tomorrow’s healthcare—right now.
BWF can assist your AMC with insights and tools on how to overcome these challenges when cultivating philanthropic donors and help you harness the power and innovation of an academic medical center. Please reach out to Kara Wagner, associate vice president, or Elizabeth Dollhopf-Brown, consulting partner. It’s a privilege to help.